BURLINGTON, ON November 12, 2011
Going out on a high note is the best way to leave the stage – which is what Mayor Goldring is doing with his Inspire series when, Andre Picard, Health reporter and columnist for the Globe and Mail will be the featured speaker at the last of the 2011 series the Mayor instituted during his first year in office.
Attendance has been good and it will grow as people get used the idea of speakers coming to Burlington with new ideas that stimulate and offer new and different perspectives and begin to recognize the quality of the speakers the Mayor is bringing to the city.
The series started with Christopher Hume, Architectural reporter and columnist for the Toronto Star who told his audience that McMaster University`s behavior in the way they handled building of their Burlington campus on the South Service Rd., was a moral outrage. There was no doubt in his mind where he stood on all this.
That was followed by Gil Penalosa, a passionate advocate for improving quality of life through the promotion of walking and bicycling, and of parks, trails and other public spaces as great places which foster vibrant cities with healthier communities and happier residents.
Penalosa earned a Master in Business Administration (MBA) from UCLA’s Management School. Following years of private and public sector senior managerial experience, the Mayor of Bogotá, Colombia (pop. 7 m), appointed him Commissioner of Parks, Sport and Recreation for the city.
Penalosa led his team to design and build over 200 parks, of which the best known is the Simón Bolívar (360 hectares). They were also successful in opening 91 kilometres of car-free city roads on Sundays, the Ciclovia, where over 1.3 m. people come out weekly to walk, run, skate and bike. They also created the Summer Festival, with over 100 events in 10 days and more than 3 million people attending and since the first year has become the main recreational event in the country.

Tom Rand, author of Kick was the third speaker in the Inspire series. He advocated ways to reduce our carbon footprint.
Penalosa was followed by Kick author Tom Rand, a successful software entrepreneur who survived the dot com bubble in 2000. Rand now focuses his efforts on carbon mitigation and is active in Cleantech venture capital, technology incubation and commercialization plus public advocacy. Rand is the Cleantech Practice, Lead Advisor at the MaRS Discovery District in Toronto and sits on the board of a number of clean energy companies and organizations, including Morgan Solar.
One speaker was on the platform the night of an NHL playoff game – but the crowd was still good – in the 150 + range.
The series have in the past been held at the Ron Joyce Centre of the McMaster DeGroote School of Business on the South Service Road. The Mayor has decided to keep the business in the family and this last event for the 2011 series will take place in the Community Theatre of the Burlington Performing Arts Centre. The event starts at 7 pm – the Mayor`s office likes to get a handle on possible attendance – the room holds just over 200 people.
Now – the speaker – Andre Picard.
Picard is the Globe and Mail’s public health reporter and columnist who was recently named the Conference Board of Canada’s CIBC scholar-in-residence.
The program has funded scholars since 2005, enabling them to carry out research on issues that resonate throughout Canada. Picard’s research topic is The Path to Health Care Reform: Policy and Politics.
“He’s the top health journalist in the country,” said Anne Golden, president and CEO of the Conference Board of Canada. “He’s able to cover both the policy issues and the politics because he’s been so engaged on the whole range of issues around all our health-care systems.”
The College of Family Physicians of Canada named Picard a recipient of its 2011 CFPC/Scotiabank Family Medicine Lectureship Award.
Mr. Picard has been recognized for years as one of the country’s top public policy writers. His books, Critical Care: Canadian Nurses Speak for Change and The Gift of Death: Confronting Canada’s Tainted-Blood Tragedy, were best-sellers.
Among Mr. Picard’s previous awards are the Michener Award for Meritorious Public Service Journalism, the Canadian Policy Research Award, the Atkinson fellowship for public policy research and the Centennial Prize of the Pan American Organization. He was named Canada’s first Public Health Hero by the Canadian Public Health Association and was honoured as a champion of mental health. He is a four-time finalist for the National Newspaper Awards.
Picard said being named the CIBC scholar-in-residence at the Conference Board will give him new opportunities and called it “a nice challenge.” “This one allows me to do some journalism – some long-form journalism,” he said. “It allows you to do the work that you usually do but in a different way and more in-depth.”
In a recent column Picard had this to say:
Andre Picard, Globe and Mail columnist and perhaps the most prominent speaker the Mayor has brought to Burlington. His views on our health system may include some comments on the Joseph Brant Memorial Hospital. He will be a very direct speaker.
One of the fundamental structural problems in Canada’s health system is the lack of a clearly identified front door.
Put another way, there is no place where patients can routinely go to access the care they need promptly and efficiently and that tracks them throughout the health-care “journey.”
Traditionally, we have depended on family physicians to serve as that home base. Almost 30 million Canadians have a family doctor, but roughly four million others have none. Still, even for those with a regular caregiver, prompt appointments are hard to come by and same-day access – the gold standard – is a rarity.
So the de facto entry point into the system all too often becomes the emergency room (where patching and dispatching, and long waits, are the norm) or walk-in clinics (tremendous money-wasters that specialize in passing the buck back to ERs or family doctors).
Using these inappropriate points of access is the equivalent of entering your home by clambering up the fire escape or crawling in through a basement window, only to find that the door into the main floor is locked and you have to start over again.
It’s a terribly inefficient and expensive way to deliver health care. Among other things, when there is no front door, there is no real gatekeeper and, with the proliferation of ever-more-expensive drugs and technologies, the gatekeeper function has become more essential than ever.
Worse yet, regardless of what door patients use to enter the health system, there is little continuity in their care.
One of the principal reasons for this disjointedness is the lack of electronic health records. If someone has a heart attack and ends up in the ER, or is prescribed antibiotics at a walk-in clinic, or gets to see a specialist, his or her family doctor is unlikely to know.
This situation is not new.
The Inspire Series is one of the best things the Mayor has done for the city. It ranks right up there with his decision to tough it out and continue with the building of The Pier.
Primary health reform has been talked about for decades. In fact, with the publication of the Lalonde report, a ground-breaking document prepared by health minister Marc Lalonde in 1974, Canada became a world leader in the concept of primary care (but sadly not in the practice.) Every one of the dozens of health commissions since has dedicated a good chunk of its recommendations to the need for primary-care reform.
In the 2004 Health Accord, the provinces received $800-million to bolster primary care, but it was overshadowed by the politically motivated focus on reducing surgical wait times, where billions were invested to produce modest results.
The good news is that there has been a lot of progress of late on the notion that every Canadian should have a clearly identifiable primary-care provider for preventive care, sickness care, and some quarterbacking and follow-up when a patient needs acute care.
In the 21st century, this kind of care can’t be provided by a single physician à la Marcus Welby.
Today’s patients require episodic care occasionally, but mostly they need chronic care. Consider that 81 per cent of people over the age of 65 have at least one chronic health condition such as heart disease, diabetes, chronic obstructive pulmonary disease, etc. For the most part, they need a team to provide health care, not a single physician.
Thankfully, in recent years, there has been a significant shift to providing primary care using interdisciplinary teams. Alberta has Primary Care Networks; Ontario has Family Health Teams; Quebec has Family Medicine Groups and; most other provinces have variations on these names with similar philosophies.
We shouldn’t forget either that excellent primary care has been offered for decades by CLSCs (community health clinics) in Quebec and Community Health Centres in Ontario, but these pioneering initiatives have always been chronically underfunded.
But the process needs to be accelerated and valued. And, practically, that means shifting resources from acute-care hospitals to community-based primary-care practice.
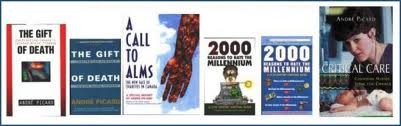
Picard is a prolific writer who works from his home in Montreal as the Globe and Mails Health columnist. He has been given some very significant awards for his work.
The notion of creating a clear front door into the health system got a significant boost recently in a report from the College of Family Physicians of Canada, which represents the country’s 35,000 family doctors. (Canada has another 34,000 physicians in specialties other than family medicine.)
The CFPC calls for a model that has as its foundation a concept called the “Patient’s Medical Home.” The PMH is described as a family practice that serves as the “central hub for timely provision and co-ordination of a comprehensive menu of health and medical services patients need.”
The PMH is, naturally enough, centered around the family doctor (after all that’s who the CFPC represents), but, to its credit, the group fully embraces the need for interdisciplinary care, the belief that a patient requires a team or network of caregivers, including nurses, pharmacists, physician assistants, and other health professionals, located in the same physical site or linked virtually from different practice sites throughout the community.
The report also makes some key points that are not emphasized nearly enough in our continuing discussions about health-care reform. To wit:
The foundation of good healthcare is good relationships between providers and patients, and among providers;
Timely access to both prevention and treatment is an essential component of good health care, and Canada’s waits are among the worst in the world;
Patients themselves need to be active participants in their care. They need to take responsibility, not just be passive recipients of care;
Continuity of care has to be a priority because it is in the transitions – from the family doctor to the specialist, from the ER to the ward, from hospital to home, etc. – where all the bad things happen.
In Canada, we have a terribly knee-jerk reflex when responding to problems: We throw more money and bodies into doing more of the same, no matter how inefficient.
With primary care, the opportunity for reform lies in actually doing things differently and ensuring that patients have access to the right care, at the right time, from the right professional.
That can’t even begin to happen if there is no front door, no medical home for them to call their own.
Burlington is in for a treat. The Community Room at the Performing Arts Centre has seating for just over 200 people – this could be a SOLD OUT event, which by the way is free.